
How to Get into Oncology Training in the NHS
04 Oct, 202316 Minutes
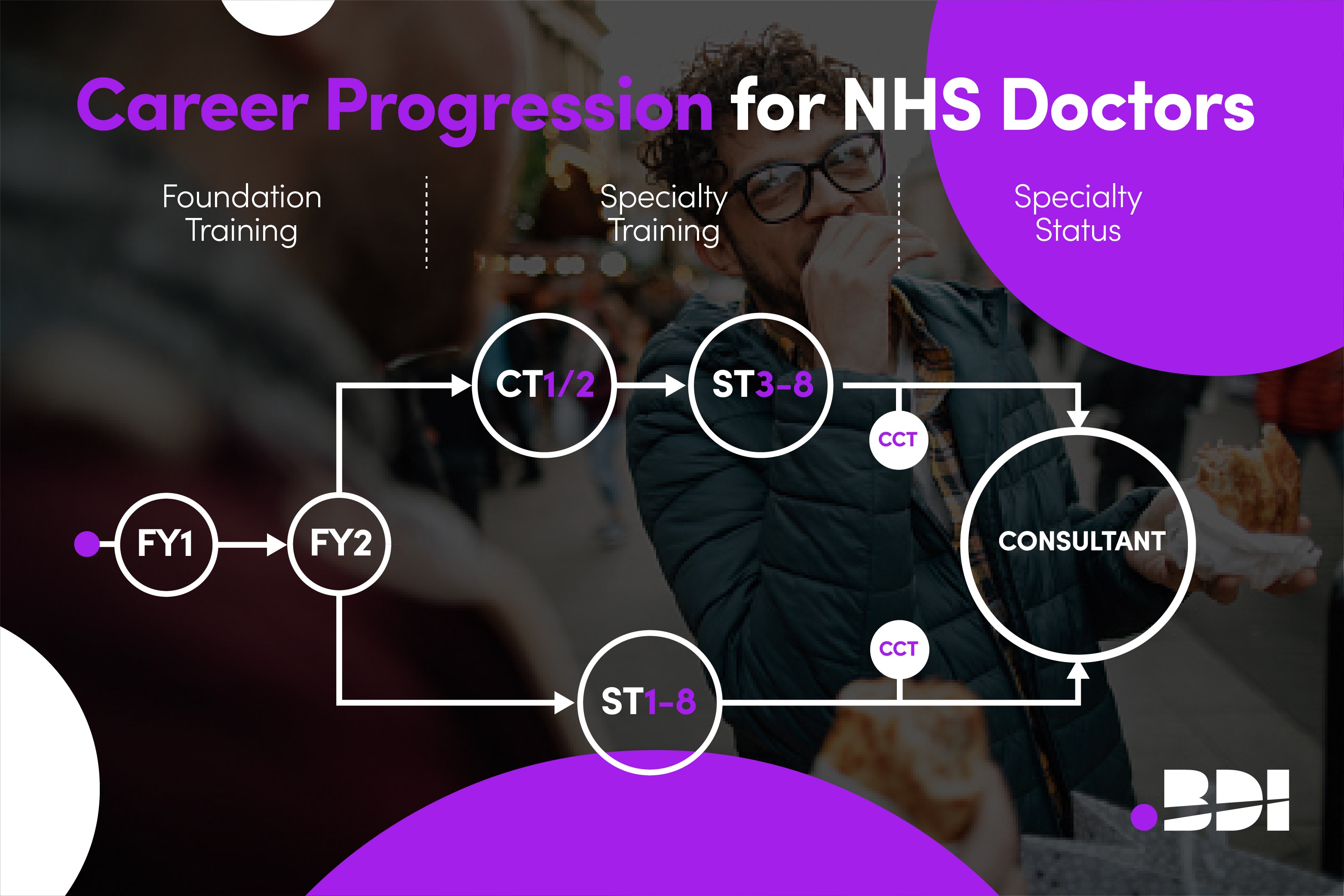
The road to specialist NHS training in Oncology is a somewhat complex one. That is especially true for IMGs who aren’t familiar with the NHS system. You may have a dream of becoming an NHS oncologist but don’t know the first place to begin! Don’t worry – we’ve got you covered with this guide.
Despite being competitive and complicated, getting into oncology training is an excellent choice, as it provides a pathway to working at the Consultant level in the NHS, which is prestigious accolade in the UK but also around the world. Plus, the NHS offers an excellent training system where you get paid a really good salary whilst working your way through a highly specialised system and gaining a wealth of knowledge and experience.
Are you ready to begin oncology training in the NHS? Read on to learn how to do so as an IMG.
Getting GMC Registered
GMC registration is a must-have if you want to work as a trainee oncologist (or any kind of doctor in the UK). There are several documents you need for this stage, including your passport, certificate of good standing, proof of internship, and evidence of knowledge and skills. If you’re at this stage you might find it helpful to read our article on How to Get GMC Registration for IMGs.
How you prove your clinical knowledge and skills is really important. Many IMGs take the PLAB route, which generally grants you access to NHS posts at level ST1/CT1. However, taking a GMC-accepted postgraduate qualification like MRCP grants you access to non-training roles at level ST3+.
Working in a Service Role
As an IMG, you will usually need to work in a service role/non-training role for at least a year before entering specialty training. Doing this will give you the experience to secure a training post later. During this time, you’ll gain a lot of experience working in NHS hospitals, helping you to build your portfolio and compete with all the other oncology specialty training applicants.
The service post level you start at depends on your experience. Many IMGs start in a role equivalent to ST1/CT1. To get into these levels, you’ll complete PLAB for GMC registration. If you want to start a non-training job at a higher level, you can use MRCP(UK) to do so. These non-training jobs are where BDI Resourcing can help if you’re ready to start your job search.
Completing the CREST Form
After a year or more in a non-training post, you can begin the next stage of the route to medical or clinical oncology training, which will either be ACCS in acute medicine or CMT. To pursue this next step, you’ll need to get the CREST form signed off (the alternative certificate of foundation competencies). The form proves your success and competence as a foundation doctor. The form involves completing a checklist and including particular documents (like GMC registration) and then getting it signed by somebody registered with a medical regulatory board who has worked with you for three months during the last three and a half years. A UK Consultant works very well here and the following video sets our 10 tips to for completing the CREST form:
Keep in mind there is an exception to the CREST form: if you completed an FY2 post as an IMG, you’ll receive the FPCC and can use this to move on to specialty training. Also, if you started at an ST3+ level role, you’ll complete the Alternative Certificate to enter Higher Physician Specialty Training instead, which provides access to higher specialty training.
CMT or ACCS in Acute Medicine
Both medical and clinical oncology are uncoupled specialties, which means there are two recruitment processes – one for core-level training and another for higher specialty training. The two options for the core level training years are either a three-year acute common care stem programme or a two-year core medical training programme, and these work for either medical or clinical oncology higher specialty training programmes.
CMT
CMT stands for core medical training. It’s a two-year programme NHS trainees take to pursue ST3 specialty training later (including in oncology). During this time, you’ll work in rotations, meaning you’ll get experience in different places in a hospital. The pr`ogramme will always include a rotation in acute medicine; plus, you can get experience in certain medical specialties during the two years. At the end of CMT, you’ll need to get a sign-off to prove you’ve met all competencies.
ACCS in Acute Medicine
The other option is taking a three-year Acute Care Common Stem programme in acute medicine. This is a route to oncology training that focuses primarily on acute care. Like CMT, you’ll spend your time doing hospital rotations (lasting between four and six months) to build experience and gain competencies. By completing this programme, you prove you have the skills necessary to move on to higher specialty training.
Whilst completing either CMT or ACCS in Acute Medicine, you’ll need to pass MRCP(UK), which we’ll go into in the next section.
MRCP(UK)
To apply for higher specialty training in oncology, you’ll need to pass all parts of MRCP(UK). You will do this during your internal medicine training years, ensuring you pass part two and PACES before applying for ST3+ positions. This will grant you the Membership of the Royal College of Physicians.
The MRCP(UK) exams come in three parts: part one, part two, and PACES. Parts one and two involve multiple-choice question papers, whereas PACES is a practical examination that you’ll need to complete in Manchester, UK. Upon its completion, you can begin applying for higher specialty training.
It should be noted that some IMGs do MRCP(UK) before they work in the UK. These IMGs will already have a lot of experience from overseas, and they will use that to gain a Membership of the Royal College of Physicians and start their NHS career at a higher level. If you do this, you will prove your high skill level and be able to apply for either clinical or medical oncology training straight at ST3 level, bypassing CMT/ACCS.
Clinical vs. Medical Oncology
When it comes to specialising in oncology as a trainee doctor, you have two options in the UK: clinical vs. medical oncology. Getting into either of these programmes requires the same years of core training, either in CMT or ACCS, and you must decide which one you’ll take before applying for higher speciality training. While there are some similarities between the two specialties, there are also some stark differences, so choose wisely. Our full guide on What to Expect Working in Oncology in the NHS takes you through your options in full depth and the following offers a handy overview.
Clinical Oncology
Clinical oncology focuses on the techniques of radiotherapy and chemotherapy to treat and manage cancer. If you went into clinical oncology training, you’d be responsible for determining the best way to treat cancer - either through chemotherapy or radiotherapy - on an individual level, depending on location or severity.
While studying clinical oncology, your goal will be to complete your CCT, which allows you to get on the specialist register as a clinical oncologist. Keep in mind there are no subspecialties within the clinical oncology specialty, but you will focus on particular cancers in the later years of training.
Medical Oncology
Medical oncology focuses on diagnosing, assessing, and treating different types of cancers. A lot of medical oncologists’ work comes from assessing patients and performing tests. It also involves providing advice and further treatment for a patient – much like clinical oncologists, medical oncologists determine the best ways to manage the cancer. Unlike clinical oncology, medical oncologists may involve surgical treatments.
Like clinical oncology, there are no subspecialties for getting a CCT in medical oncology. However, there are different types of cancers or diagnostic techniques you can choose to focus on during training.
Dual Training Programme
There is also the option of pursuing a dual training programme. These are very specific programmes that allow you to train in two specialties at the same time – for example, medical oncology and palliative care. At the end of dual training, you can get a dual CCT that proves you pass all competencies for each of the specialities.

Applying for ST3+ Oncology Training
Once you have completed your core-level training years and MRCP(UK), you can finally start applying to oncology positions in the NHS. Congratulations!
Of course, this isn’t the end of the road. These posts are extremely competitive, and you’ll still have four years of higher specialty training in oncology to complete before you can become a Consultant oncologist. Still, these ST3+ posts do offer higher levels of responsibilities, a lot of education/training around oncology, and an attractive salary (you don’t need to pay anything for this training).
So, how can you increase your chances of getting an oncology training post in the NHS? By understanding the application process and sending a stellar application. Here’s how you can do that:
Ensure You’re Eligible
There’s no point in applying for an ST3+ oncology specialty training position if you aren’t eligible. You’ll need to meet the requirements, which include:
- Completing MRCP(UK)
- Meeting experience requirements
- Being GMC registered
- Meeting core competencies
- Proven English language capabilities
Understand How Your Application will be Assessed
The NHS specialty training application process goes through three stages: longlisting, shortlisting, and interviewing. At the longlisting stage, you’ll be assessed based on the eligibility criteria you meet (such as your qualifications and experience). At the shortlisting stage, the NHS will go through eligible candidates more closely, assuming there are more eligible applications than there are vacancies. Finally, there’s the interview stage, which we’ll go into a little later.
Build Evidence
One of the biggest parts of your application will involve building evidence, which you’ll demonstrate in the self-assessment part of the NHS specialty application. By building evidence, you’ll be able to gain more points in the self-assessment stage.
The self-assessment part of the application gives you an overall score depending on your experience and qualifications. The more you have, the better your score will be, increasing your chance of getting shortlisted. Overall, there are 48 points in total available. It’s crucial not to over-claim on this part, as you will later need to supply evidence to back up your self-assessment.
Use Oriel to Apply
You might be wondering where you can apply for these positions. You can use Oriel, a digital recruitment system that allows all UK candidates to apply for jobs while keeping up with their applications. It will list vacancies from around the UK, so you have a high chance of finding an oncology training position that works for you.
Verifying Evidence
You’ll only need to verify your evidence (supplying documentation) after the applications close. This will come before being invited to an interview. Here, it’s important to show organised evidence as the interviewers only have a short amount of time to go through it before interviewing. You should also avoid uploading evidence that isn’t relevant; only supply evidence of achievements you have claimed in the application process. You will be scored on the organisation of your evidence, as well as whether you have over or under-supplied.
Once you have submitted your application, you’ll need to wait for the next stage, which is an interview. You’ll find out whether you have been invited for an interview through email or your Oriel account.
One thing to remember while applying for ST3+ oncology positions is the difference between medical and clinical oncology training. You can choose to pursue either at this stage, so it’s worth researching what each specialty entails. Generally, medical oncology covers diagnosing and assessing patients with cancers, while clinical oncology works more closely with treating cancers with radiotherapy, chemotherapy, and other radiological techniques.

Interviewing for an Oncology Training Position
Being asked to interview for an oncology training position is a fantastic achievement. So, what next? Naturally, you want to increase your chances of getting the post, and knowing what to expect is paramount for that.
Oncology Interview General Format
For the NHS oncology interview, you’ll have to complete two stations. Each station has four questions – you get five to seven minutes to listen to and answer these questions. Overall, expect the interview to last up to half an hour.
Station one includes clinical scenarios and professional and governance questions; station two includes academic research and suitability & commitment questions. For each question, you’ll be graded on a score between 1 and 5, with one being poor and five being excellent. An overall score of three would be satisfactory.
Preparing for the Interview
You can’t exactly revise for an interview, but you can familiarise yourself with the format and look up common oncology questions. NHS interviews have several types of questions, such as ethical scenarios, clinical scenarios, and skills and experience questions. You should familiarise yourself with these formats and read and prepare for the most common oncology questions, such as “Why did you decide to go into oncology?”. You should also prepare some questions for the interview panel at the end. Our downloadable guide to Oncology Interview Questions contains loads of example questions for you to work through in preparation.
In terms of documentation, you usually won’t need to supply any other documents on the day other than proof of ID (usually your passport).
Meeting Technical Requirements
NHS interviews take place online. As such, it’s important to meet technical requirements on the day. That means setting up a working microphone and camera, ensuring a stable internet connection, and keeping a distraction-free background and environment.
How Competitive is Oncology Training?
So, how competitive is oncology training? Going into this specialty, it’s a good idea to know how likely you are to find a job. The truth is oncology specialty training is highly competitive, so it might take you several job applications to land a role.
The competition ratio for each NHS specialty can be found here. There, you can see that in 2022, ST3 clinical oncology roles had 194 applications for 115 posts. For ST3 medical oncology, there were 214 applications for 88 posts. So, while oncology is competitive as a whole, medical oncology is more competitive than clinical oncology.
Application and Offer Dates for Oncology in 2024
You likely want to know when you can begin applications for higher specialty training in oncology. Here is the recruitment timeline for 2024:
- Adverts for Specialty Posts: Released by 5pm 15th November 2023.
- Applications Open: From 10am 16th November 2023 until 4pm 7th December 2023.
- Longlisting and Shortlisting: From the time of application until seven days before the interview.
- Interviews: From 2nd January 2024 to 16th April 2024.
- First Offer: 5pm 18th April 2024.
- Offer Holding: 1pm 23rd April 2024.
- Offer Upgrade: 1pm 24th April 2024.
- Interview Feedback: 5pm 25th April 2024.

What to expect During Oncology Training
Both clinical and medical oncology training programmes last a total of five years. During that time, it’s recommended that you pursue a higher degree in a UK university to improve your training and skills. Once you’ve joined a university, there’s a lot you can do to boost your training and skills, such as:
- Joining oncology research projects
- Publishing essays
- Taking on teaching/management roles
- Completing a PhD or MSc
Getting a higher degree (such as a PhD or MSc) isn’t required but is recommended. However, there is one qualification that is required to complete CCT in clinical oncology: FRCR. During your time in clinical oncology training, you will work towards obtaining the Fellowship of the Royal College of Radiologists for Oncologists. These exams come in three parts and test your skills and knowledge as an oncology doctor, ensuring you meet all competencies to practice independently. Only once you have passed the final FRCR exam can you complete oncology training (whether in medical or clinical oncology).
What Happens After Oncology Training?
Getting into oncology training is an excellent achievement. What happens once you complete ST3-8, though? At that stage, you can get your CCT (certificate of completion of training) to join the specialist register. If you did medical oncology, you will need to complete (and pass) the Specialist Certificate Exam (SCE) before getting your CCT, though. Keep in mind that you’ll also need to have passed all the CiPs given by the Royal College. Doing so enables you to apply for consultant oncology positions, which are senior NHS positions that pay a very competitive salary. For many IMGs and UK doctors alike, this is the ultimate goal.
Of course, you can also go into further training after getting on the specialist register! While there are no specific subspecialties, you can go into specific areas of oncology, such as gastrointestinal tract cancers, paediatric oncology, palliative care, and urological cancers.
In a case where you have completed specialist training in oncology overseas and have a lot of experience and knowledge behind you, you can even get on the specialist register through CESR/ Portfolio Pathway. The certificate of eligibility for specialist registration is a lengthy process, and you’ll need to submit tons of evidence to prove that you can work independently as an oncologist. You should only consider it if you are already a specialist oncologist with the evidence to back that up. The other option is beginning at the ST1/CT1 level, which will also take a lot of time and require a lot of work.

CESR / Portfolio Pathway for Oncology – An alternative Option
If you are already working at a senior level or have completed a training programme in your home country then going back through the UK training system might feel like a step backwards. That’s where CESR / Portfolio Pathway comes in. You can use your overseas experience to evidence your capabilities of working at a Consultant level for an alternative route to specialist registration. It’s a long process that requires a lot of evidence to complete however we’ve simplified it by creating a full guide on How to Get CESR in Clinical / Medical Oncology.
In Summary
Getting into specialty oncology training in the NHS is no walk in the park. For most IMGs, it means joining the NHS in a service post and completing ACCS in acute medicine or a CMT programme before applying for oncology higher training posts. Even then, the competition is very high, so you must thoroughly understand the recruitment process to increase your chances of landing one of the oncology training places.
Don’t let the difficulty put you off, though – oncology (whether medical or clinical) is an excellent specialty and can prove a fantastic, rewarding specialty for your NHS career. Just be aware that you’ll need to put in a lot of years and dedication to make it happen.
BDI Resourcing – Supporting IMG Oncologists
At BDI Resourcing we are in the fortunate position of having worked with over 100 NHS Trusts to provide them with thousands of international doctors. Our candidates have only given 5-star reviews so we’re in an excellent position to help you too. Remember that if your long term dream is NHS training then that journey often starts with a non-training or service post. BDI Resourcing work with a number of the leading Cancer Centres around the UK so we can connect you to those for your first role. Get in touch with our Oncology team to find out more.



